Background
Patients with coronavirus disease 2019 (COVID-19) frequently have hematologic derangements prompting specialty consultation. Management of such derangements remain complicated by a nascent evidence base. Our primary objective was to identify the main reasons for hematology consultation in patients with COVID-19 at a university medical center in New York City during the initial peak of the pandemic in 2020. We sought to determine the hematologic parameters that may affect patient outcomes and to provide recommendations to improve clinical practice.
Methods
We completed an observational study of consecutive hematology consultations requested between March 16 and April 27, 2020, for adult patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection admitted to a university medical center. Diagnosis of SARS-CoV-2 infection was confirmed via reverse transcriptase polymerase chain reaction of nasopharyngeal swabs. Using the electronic medical record, we collected demographic information, reasons for consultation, laboratory parameters relevant to hematology, diagnoses, recommendations, and outcomes. Descriptive statistics and Wilcoxon rank sum tests were used for data analysis.
Results
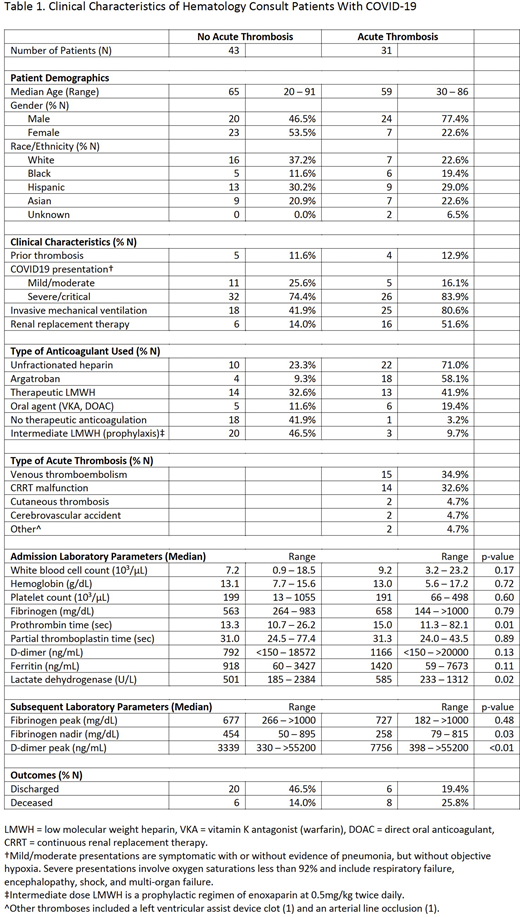
A total of 74 hematology consultations for unique patients were completed during the 6-week study period. The most frequent reason for consultation was for anticoagulation recommendations in the setting of suspected or confirmed acute thrombosis (46%), followed by requests for management advice regarding cytopenias (24%) and other laboratory abnormalities including elevated D-dimer and thrombocytosis (22%). As shown in Table 1, the observed rate of acute thrombosis (35 events in 31 patients, 41% of study population) did not fully account for the observed rate of therapeutic anticoagulation use (55 patients, 74% of study population). Only 5 of 25 patients without diagnosed thrombosis who received therapeutic anticoagulation during admission had a confirmed prior indication for anticoagulation such as atrial fibrillation or venous thromboembolism (VTE).
Objectively documented VTE (15 events in 15 patients) was the most common type of thrombosis, followed by thrombotic occlusion of continuous renal replacement (CRRT) circuits (14 events in 14 patients). Two cases of cutaneous thrombosis were also observed, identified on biopsies of retiform purpuric lesions. Unfractionated heparin was the most frequently utilized parenteral agent for therapeutic anticoagulation. Interestingly, a significant number of patients received argatroban (22 patients), despite a comparably low rate of evaluation for heparin-induced thrombocytopenia (10 patients tested). Occluded CRRT circuits accounted for the majority of argatroban use (12 patients), followed by thrombocytopenia (10 patients), including 3 of the 4 patients without thrombosis who received argatroban.
Patients objectively diagnosed with acute thromboses had higher levels of D-dimer (median 1166 ng/mL) and ferritin (1420 ng/mL) at initial admission relative to patients without thromboses (median 792 ng/mL and 918 ng/mL, respectively). Notable differences in peak D-dimer (median 7756 ng/mL vs 3399 ng/mL) and fibrinogen nadir (258 mg/dL vs 454 mg/dL) were also observed. Statistical analysis via Wilcoxon rank sum test (p-values reported) corroborated the presence of differences in the distribution of laboratory values between the two groups. Acute thrombosis was also associated with a lower rate of hospital discharge and a higher rate of mortality during the study period (Table 1).
Conclusions
Hematologic consultation patterns during the peak of the COVID-19 pandemic in New York City were characterized by frequent requests for assistance with anticoagulation management, further corroborated by a high incidence of acute thrombotic events. The early suspicion of thrombosis and laboratory derangements on hospital admission appeared to drive widespread use of empiric anticoagulation. Atypical events like CRRT circuit occlusions and concurrent hematologic abnormalities like thrombocytopenia likely underlie the notable use of argatroban in this cohort. These observations underscore the importance of prospective randomized controlled studies to address anticoagulation strategies and routine hematologic laboratory monitoring in hospitalized patients with COVID-19.
De Sancho:Sanofi Genzyme:Membership on an entity's Board of Directors or advisory committees;Apellis Pharmaceuticals:Membership on an entity's Board of Directors or advisory committees;Bio Products Laboratory:Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal